Understanding Managed Care
IPEHN presents its version of "Managed Care 101" to soothe the pain and confusion caused by today's healthcare environment
BY SANDY BURK
Spurred by voter
outcry, state and
Federal governments
have begun to
mandate reform in
managed care. The
most visible example
is a guaranteed two-
or three-day hospital
stay for women and
newborns following
delivery.
Over the years, the rising costs of healthcare—resulting from a rapidly changing healthcare system—have
translated into similarly increasing insurance premiums.
By the late 1980s, annual increases for health insurance
premiums outpaced inflation, reaching as high as 19
percent at its worst point. Employers were finding that
providing health insurance benefits was becoming too
expensive.
In response, health insurers introduced "managed care," a series of
options that manage the cost of
healthcare and, thus, help employers keep premiums under control.
Managed care quickly became the
norm as enrollment in all types of
managed care plans at large employers rose from 6 percent of covered
workers in 1994 to 73 percent in
1995.
This explosive growth gave rise to
a plethora of managed care plans,
some of which unscrupulously placed
quality in a back seat to cost. As a result, "horror stories" about managed care plans, particularly health maintenance organizations (HMOs), appeared in the media. Spurred by voter outcry, state and federal governments have begun to mandate reform in managed care.
The most visible example is a guaranteed two- or three-
day hospital stay for women and newborns following
delivery.
Unfortunately, the horror stories and mandates have
caused many people to equate managed care with less
care. But that's like throwing out the baby with the
bath water! Through careful planning and investigation by employers, managed care can and does provide
quick access, quality of care and competitive cost.
What is managed care?
|
|
It's important to remember that "managed care" is a
concept. It's not an HMO or any other kind of specific
plan. The concept can best be described as a broad spectrum of cost controlling options designed to coordinate the financing and provision
of healthcare to produce high-quality healthcare for the lowest possible
cost.
Managed care has two key components: utilization review and healthcare provider networks/ arrangements. Utilization review
serves to screen against medical tests
and treatments that are unnecessary.
The screening is done by the insurance company's medical staff (using
nationally accepted standards of medical practice) to
make sure that the treatment is medically necessary
and will be delivered in the most cost-effective manner
possible. To accomplish this, techniques such as preapproval of hospital admissions and surgeries, review
of treatment received, and case management for patients needing high-cost care are employed. Utilization
review techniques arc widely used today in varying degrees in most insurance plans.
|
It is the second component—health provider networks/arrangements—that is most misunderstood and
July/August 1997 /21
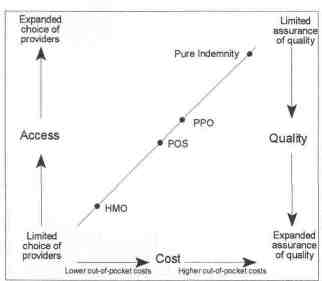
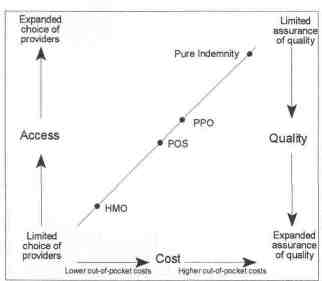
viewed with trepidation. Managed care networks represent a variety of arrangements with healthcare provider
groups which enable insurance providers to have more
control over costs. While these arrangements are constantly evolving, they can be succinctly categorized into
three basic plans: health maintenance organizations
(HMO), preferred provider options (PPO) and point of
service (POS). These plans are basically contracted arrangements which establish alliances between insurance
companies and a select group of doctors and hospitals
who agree to provide services at a discounted or fixed
cost. HMO, PPO, and POS plans all offer employers
the ability to control their healthcare expenditures. They
range in a continuum which balances cost against freedom of choice among healthcare providers.
At one end are the traditional indemnity plans which
are fee-for-service arrangements. In this arrangement,
a premium is charged for each covered person. In return, covered individuals may use any doctor, hospital
or other healthcare provider of their choice and expect
to have medical expenses reimbursed. These plans typically have the highest premiums.
+HMOs
At the other end of the continuum are HMOs, the
most tightly controlled of managed care arrangement
with the lowest premiums (see chart on page 23). HMO
plans are made up of a specific network of doctors and
hospitals who agree to care for a group of patients for a
fixed cost per member per month (capitation) and assume responsibility for providing all necessary healthcare
for a fixed premium payment without regard to the
actual cost of providing these services. The HMO establishes a network (or panel) of participating doctors and other providers who meet the plan's criteria
for participation, including licensure, training, and practice patterns. The treatments that are covered are much
broader than those covered under the traditional indemnity or PPO plans. Preventive care such as wellchild care and routine physicals are cornerstones of these
plans. Some HMOs require a deductible for hospital
charges and almost all require a minimal co-payment
for physician office visits.
Although HMOs offer the greatest control of
healthcare costs and thus the lowest premiums, they
do so at the expense of freedom to use a provider of
choice. HMO members are required to use a plan doctor or hospital in order to have their expenses covered,
Treatment provided outside of the network is not covered at all. Use of a primary care physician (PCP), also
known as a "gatekeeper," to oversee all care and treatment is common and hospitallzation or treatment by a specialist requires a referral by the PCP in order to be
covered.
While many people see the gatekeeper approach as a
negative, there are definite advantages inherent in this
process. Specifically, there is more emphasis on the patient/physician relationship, preventive services are provided, and the determination of the appropriateness of
treatment and site of care is performed before the treatment is received rather than afterwards which optimizes
the likelihood of a successful outcome. All parties—
patient, health plan and providers—benefit under this
methodology.
+ PPOs
PPOs plans came next in the evolution of managed
care and were developed to take advantage of the cost controlling strengths of HMOs while providing more
freedom of choice. PPOs retain the characteristics of
22/ Illinois Parks and Recreation
the indemnity plans including freedom to choose a provider outside the network who will be reimbursed on a
fee-for-service basis. However, PPOs offer a higher co insurance reimbursement for services performed innetwork This steers patients to specific doctors and
hospitals who have contracted with the PPO plan to
provide discounted fees and results in reduced overall
claims costs and lower overall premiums.
Park district and
special recreation
associations are
usually smaller
employers and are
not able to assume
the financial risk that
is inherent to self insurance.
+ POSs
Point-of-service (POS) plans are a hybrid of the HMO
and PPO, combining the strengths of each. In a POS
arrangement, medical providers agree to charge discounted fees. The network of hospitals and doctors is
wider than PPO networks. POS plans allows patients
to choose any doctor or hospital, but pays a larger benefit when network doctors are used. On the other hand,
POS plans provide greater cost controls than PPOs
because they function much the same as HMOs, including the gatekeeper provision. A specialist may be
used without a referral by the primary care physician
but again the coverage is reduced which increases the
employee's out of pocket cost, thus providing an incentive to stay within the network.
Traditional indemnity plans have been incorporating several of the managed care techniques in recent
years in order to contain costs: utilization review, preadmission certification, and case management for highcost chronic or catastrophic cases. The managed indemnity plans offer the least control of any of the
managed care arrangements.
Managed care arrangements are constantly evolving
because of changing economic constraints, technological advances and the social environment. As they continue to evolve, specific areas of healthcare such as
mental health (also known as behavioral health), prescription drugs, dental service and vision care often are
"carved out" and included under single-service or limited-service managed care plans. Many managed care
plans now use centers of excellence, medical facilities
that provide specialized forms of treatment for highcost chronic conditions such as organ transplants, cancer therapies, cardiac surgery. The centers are chosen
based on their outcomes and expertise, location and
willingness to negotiate discounted rates. A large number of managed care plans also provide hospice benefits
for palliative care for terminally ill patients.
|
|
Another cost-saving concept being adopted by large
employers (more than one thousand employees) is "selfinsuring," which means the employer self-funds the
cost of medical care. Employers find self-insurance desirable because of potential savings that can be achieved.
For instance, administrative costs are reduced because
employers insurers typically add risk charges onto the
administrative fees to protect themselves against adverse deviation in claims. In addition, significant cash
flow savings can be realized by taking advantage of the
lag between incurring of services and actual payment
for them. This lag can average as much as three month
and the employer is able to use the cash for an additional three months. Finally, employers have wide latitude designing the benefits of the plan and self-insured
plans typically are not subject to state-mandated benefits.
|
Park district and special recreation association are
usually smaller employers and are not able to assume
the financial risk that is inherent to self-insurance. They
may wish to have the protection of an insurance contract but may find their bargaining power regarding
options such as cost, scope of coverage and access are
limited because of their size. However, there are intergovernmental self-insured health coverage pools that
allow the typically smaller employers of the park and
recreation field to take advantage of the additional savings that large employers can generate through self insurance.
With the significant amount of money that employers spend on healthcare plans, it is important to choose
a plan that meets employees needs, does not cost more
than it should, and yet meets the employer's basic policy
objectives. To do this, employers need to make difficult decisions concerning scope of benefits and benchmarks for choosing plan administrators and provider
networks. Although the final decision rests with the
employer, assistance can be provided by a consultant or
broker.
Clearly, managed care doesn't deserve the bad rap!
In fact, it has actually served as a catalyst to provide
much broader and more proactive care. But caution is
in order when making a managed care choice.
SANDY BURK
is the benefits manager for the Illinois Park Employees Health Network (IPEHN), a
self-insured pool of 54 park districts and special recreation associations providing
healthcare coverage for its members' employees and dependents.
July/August 1997 /23